For parents of children with PDA, there is often a 'lightbulb moment' when they hear or read about PDA. They are not trying to disagree with the over-riding diagnosis of autism, but are left feeling like their child acts differently to those classic descriptions of what autism is. When these parents stumble across the suggested strategies for PDA and they work for their child, there is often some relief and a clearer understanding of how to help. This week's writer talks through some of those strategies.
My first concerns about Juliet's development were a lazy eye and delayed speech. It seems so silly how much I worried about her eye as it is the very least of my concerns now. I started being concerned about her speech around the age of eighteen months and by thirty months I was convinced she was delayed. Her tantrums seemed much more than just tantrums. People around me tried to convinced me not to worry. She had a two year check with a health visitor and all her scores fell within the 'normal' range. Before she started preschool I told them my concerns and they were reassuring that she would probably come on when she had more chance to mix with other children.
She started preschool and then about five weeks later, a week before our third child was due to be born, I was asked if I could pop in to speak to her key person. When I got there the manager and SENCO were sat down too and I knew I was about to be told it was worse than I thought. They agreed with my concerns and then some.
Autism was first mentioned to me at our first Paediatrician's appointment. I thought they were crazy - how could a child so sociable be Autistic?! A few months later I could see it. I had convinced myself that if her speech and language came on her social skills and learning would too but they didn't. There were just things about her that were different. She did make eye contact but I realised only to share enjoyment not to make requests or in conversation. Her interests were typical but obsessive and repetitive. Her behavior seemed out of control. However, she didn't seem to fit 'classic' Autism and articles describing girls with Autism sort of fit but not quite.
One day I saw something that referred to Pathological Demand Avoidance as a form of Autism and I remembered a family I had met whilst working as an SEN Officer. I thought back to things this child's mum had told me about their life and it struck me that our life was like that too. I googled PDA and the National Autistic Society's web page came up. The description of PDA described Juliet. I shared it with my husband and family and they agreed. Strategies we had naturally started using for Juliet were suggested for PDA. We had our PDA lightbulb moment.
The main thing to know about PDA is that it is described by the PDA society as an 'anxiety driven need to be in control'. A lot of Autistic, and indeed non Autistic children can be controlling. It is the level of the controlling and resulting demand avoidant behaviour that makes it PDA. My eldest tried to control things when he was younger but simple strategies quickly taught him that life won't always go your way and ways you can deal with that. With Juliet the behaviour is persistent despite lots of strategies.
Juliet is anxious most of the time and controls all she can to make herself feel better. She is expertly masking the significant difficulty she has coping with everyday life. She is easily overwhelmed by people, noise and demands. When it is just us, she feels safe and lets it all out. How much PDA affects her depends on how much anxiety and holding in she has had to deal with.
The EHCP process, though frustrating, was simple in the sense that the local authority agreed to an assessment and then a plan. They agreed with us that she would not be able to go to a mainstream school due to the level of her learning and social difficulties. A year R place was offered at our choice of special school.
It is a great school and Juliet clearly loves it. However, the demands going to school raises is very challenging for her. I can only imagine what it would be like if she were at the wrong school. She appears to cope well with all the specialist support in place but she sits on a lot of anxiety. Before school and when she comes home she lets all her pent up anxiety and frustration out.
On a good day she can be lovely, helpful and sweet. She is controlling but we get round it with many strategies we have learned along the way.
On a bad day her anxiety is high and she will control every aspect of everything. If things don't work out how she wants she can display violent and challenging behaviour mostly directed at me. She will flip out over the smallest things several times a day. At the very worst of times it is pretty much constant and she will refuse to do even the simplest of everyday tasks.
Things that might upset her are anything and everything. You can't always predict it. Things like putting toothpaste on her brush upstairs rather than downstairs, doing up the zip on her lunch box, saying she is lovely, the snow melting, someone looking at her etc etc. She sounds like a out of control, petulant child who needs more boundaries but we have tried and tried traditional strategies and they make it worse. Instead she is a 5 year old in distress and it is painful to see.
These little things that appear to cause such upset are the tip of the iceberg, the final straw of everything she has been holding in. They create a feeling of crisis and her, sometimes extreme, reaction comes from panic. We have to find ways to go along with the way she wants things where we can, doing everything to prevent distress for her and to keep everyone else safe. Things get dangerous very quickly if we don't.
Her behavior is always worse at the very start of a term, towards the end of term or after lots of changes. Her behaviour can be more flexible when there are less demands on her, especially in the school holidays. A lot of this is hidden from the outside world because of masking and because if her mood is not good we simply don't go out.
We have to be flexible with the strategies we use with her as what works changes depending on her anxiety levels. However these are things that can often work:
*Keeping everything calm.
*Backing off and and giving her space.
*Being silent
*Giving choices (2/3 max otherwise she gets overwhelmed) and then giving her lots of time to decide.
*Humour and being silly.
*Pretending you don't know what do to so she has to show you.
* Turning things into a game or race.
*Giving in to everything you can so she is more willing to go along with what she has to (we don't push her to let us brush her hair or wear socks for example because it isn't absolutely necessary but we do have to brush her teeth, attend to toileting needs, get to school).
*Timers and counting
* Visuals including a timetable (which she sometimes loves and sometimes hates!) and Makaton signing
*Using the novelty factor - people say to me 'she will settle and get used to it' but actually the opposite is usually true. If she finds something difficult she might initially cope because of it being a novelty but then struggles more and more to cope with it each time before needing a break so it becomes a novelty again.
* Understanding that Juliet sees herself as an adult, not as one of the kids.
*Anticipating things that might upset her and either not doing them or planning how best to deal with it to try to minimise a problem.
*Generally letting her think she is in control.
Triggers for behaviour:
*Not getting own way or things not happening how she expected.
*Transitions
*Changes in routine
*Being made to do things/demands
*People touching her things
*Too much choice(more than 2/3)
*Busy/loud places.
*Clothes
*Tiredness
*Sometimes there is no clear reason
I say ALL of this and know it to be true yet still I feel like a fraud: she isn't diagnosed. While we await her Autism assessment I still have that little voice saying 'what if they don't believe you?' but then also 'what if they do?'. We don't want it to be true. Not because Autism is some sort of tragedy, it isn't - there are all kinds of brilliant things about it, but because the struggle and distress we see her face everyday is heartbreaking. I know in my heart she is Autistic. It will still come as a shock when diagnosis day eventually comes.
We don't know what her future prospects are but we will do everything to make it the best it can be for her and her brothers.
NB - other important things about Juliet - she loves birthdays and Christmas, she loves running around and playing hide and seek. She loves watching Peppa Pig and princesses and Gangsta Granny. She is determined and beautiful and makes me laugh out loud. She loves her brothers. She is our lovely girl and always will be.
Thank you for reading our story.
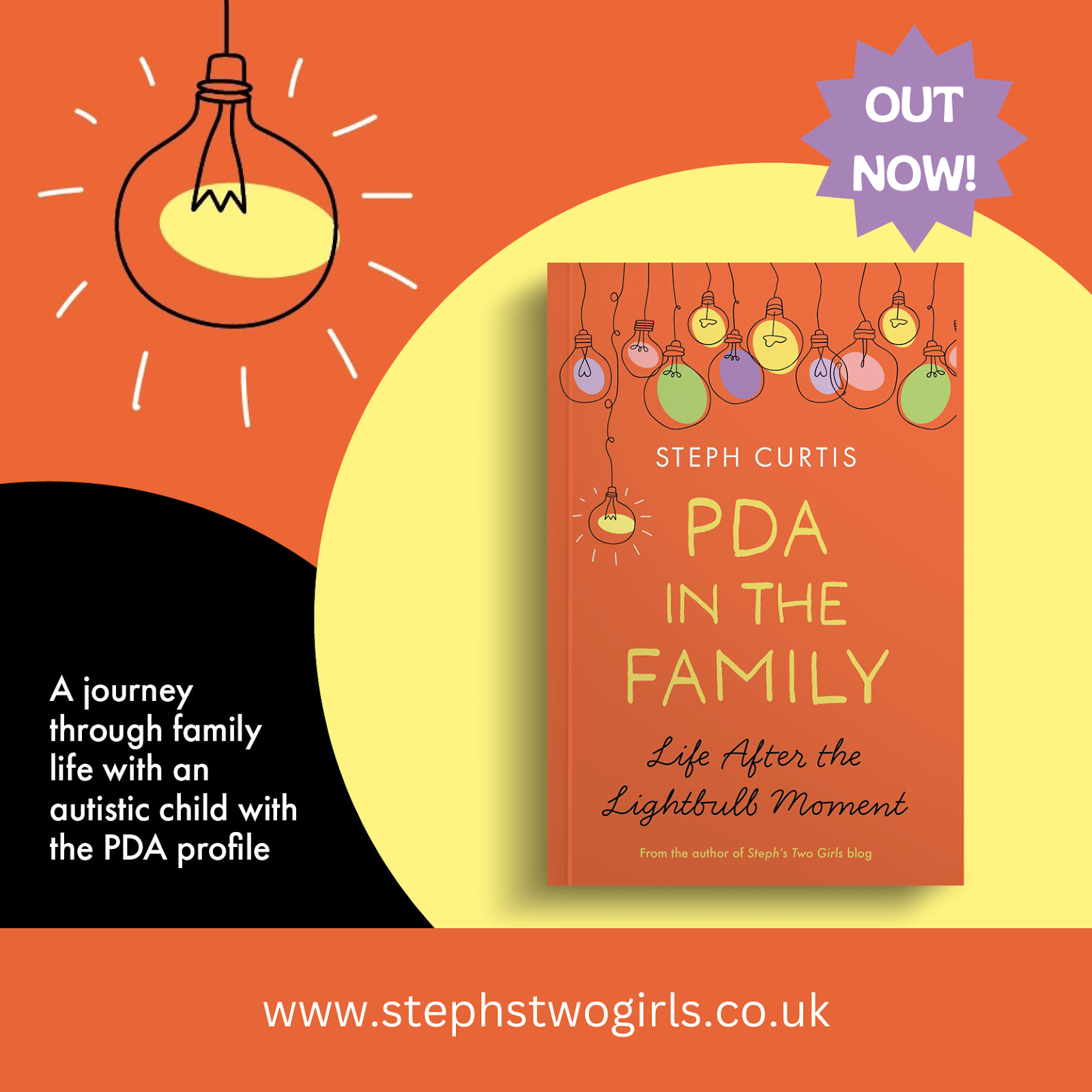
Thanks for taking the time to read. Comments are much appreciated, and sharing on social media could help get these posts to people who have still not heard about PDA. The PDA Society website has a huge range of information about Pathological Demand Avoidance.
For more reading about what Pathological Demand Avoidance is, please see 'Challenging Behaviour and PDA', and for an idea of how to help please read Strategies For PDA.
There's a chance PDA can be misdiagnosed as ODD (Oppositional Defiant Disorder) but there is a definite difference. My explanation can be found here in my post the difference between PDA and ODD.
A variety of other experiences of living with PDA can be read using the link Our PDA Story series.
If you feel up to sharing your own experiences with my readers to help spread understanding (this can be anonymously), please email stephstwogirls@gmail.com.
To find out more about our experiences, please check out our 'About Us' page. If you are looking or more information on Pathological Demand Avoidance, why not try some of these, my most popular posts?
What is PDA (Pathological Demand Avoidance)?
Ten things you need to know about Pathological Demand Avoidance
Does my child have Pathological Demand Avoidance?
The difference between PDA and ODD
Strategies for PDA (Pathological Demand Avoidance)
Pathological Demand Avoidance: Strategies for Schools
Challenging Behaviour and PDA
Is Pathological Demand Avoidance real?
Autism with demand avoidance or Pathological Demand Avoidance?
To follow me on other social media channels, you can find me at the following links or click the icons below!



















No comments:
Post a Comment
Comments are always very much appreciated and can really help the conversation go further...