The experiences below have been shared with us this week by the mother of a ten year old girl. I know that there are many others who will relate to the challenges mentioned here; school support and CAMHS certainly feature in a lot of lives where PDA is involved.
My 10 year old daughter is diagnosed with PDA and has been out of school for approximately eleven months now. We’ve been fortunate to have the support of an excellent CAMHS Clinical Psychologist and disability social worker who have supported us in ensuring school acceptance of “disability related anxiety“ so her absence isn't recorded as unauthorised and we haven't been referred to an Education Welfare Officer for prosecution. Though in my heart, I suspect the school would have preferred this, as it would deter other families in a similar situation.
It was a huge journey getting social care and CAMHS support, and that is in itself another story full of trauma, gaslighting and general gatekeeping by way of parent blaming instead of providing actual support.
Anyway I digress. I knew from when she was very young that E is autistic. She seemed to manage well and used a lot of drama, articulated her needs well. She got control of the situation and diverted others with her charm and drama offensive.
As she grew up and her peers changed it was obvious to me that her 'tool kit' no longer served as it had and she was hanging out more with the 'neurodiverse' tribe.
I took her to our local NHS paediatrician with my trolley of evidence. He diagnosed her with Autism Spectrum Condition.
As she transitioned to Year 3 and the demands increased, I noticed a difference in her functioning ability and consequences to masking through the day.
Over time her behaviour at home changed. Her resilience weakened and eventually her mental health started to crumble.
I maintained a communicative working relationship with her school, although they were adamant E 'was fine'. However, my gut told me she wasn’t. I was seeing OCD behaviours, shutdown, loss of self esteem, nihilistic thoughts and an unhappy child.
I took her to a reputable private psychiatrist for a mental health assessment and to get some guidance. This professional is someone I trust as I’d supported families in diagnosis sessions with them in the past.
The psychiatrist diagnosed E with Pathological Demand Avoidance and gave me advice on how to best mentally protect her.
Over time, not much changed in support at school as they maintained "she’s fine”. We had an EHCP in process and had obtained a really good NHS Clinical Psychologist for anxiety / school trauma support.
My child no longer felt safe to access school and was increasingly struggling to go in. I felt (while working with the education professionals) it was important for me to listen to E so I didn’t force her in. I was led by her daily. Some days we would walk to school and go home, some she would go in for a while, others not at all and eventually we didn’t even leave the house.
This was only possible as we had the great NHS CP who instructed her school that it was up to E if she felt mentally safe to go in. This was supported by our disability social worker and backed up by a whole pile of independent professionals who we had commissioned reports from to obtain her EHCP.
We are almost at the stage of getting an ASC specific small independent school named and her mental health is much better.
It’s taken months of living in a low demand, low arousal way. I have felt like I’ve been held hostage sometimes as she couldn’t leave the house. However, I recognise this is what she has needed to decompress and heal.
She’s started going to short break care provided by social services so that we can have family time out with our son. He also has a PA to take him out so he’s not forced to stay in.
Social isolation and stress are massive for parents when you have to fight like this to get very different needs met.
Thanks for taking the time to read. Comments are much appreciated, and sharing on social media could help get these posts to people who have still not heard about PDA. The PDA Society website has a huge range of information about Pathological Demand Avoidance.
For more reading about what Pathological Demand Avoidance is, please see 'Challenging Behaviour and PDA', and for an idea of how to help please read Strategies For PDA.
There's a chance PDA can be misdiagnosed as ODD (Oppositional Defiant Disorder) but there is a definite difference. My explanation can be found here in my post the difference between PDA and ODD.
A variety of other experiences of living with PDA can be read using the link Our PDA Story series.
If you feel up to sharing your own experiences with my readers to help spread understanding (this can be anonymously), please email stephstwogirls@gmail.com.
To find out more about our experiences, please check out our 'About Us' page. If you are looking for more information on Pathological Demand Avoidance, the posts below may help.
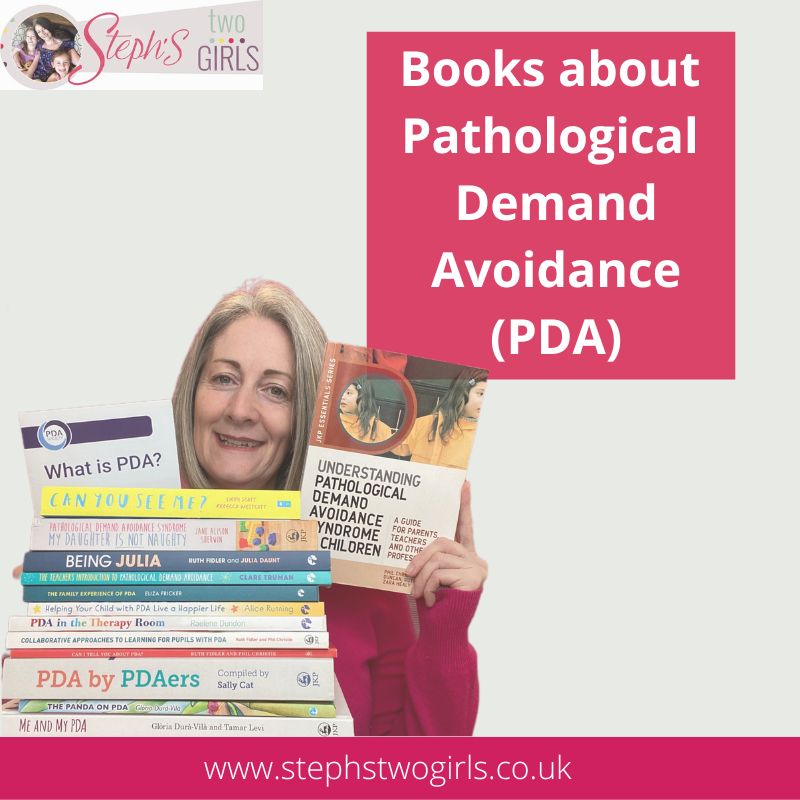
Books about the Pathological Demand Avoidance (PDA) profile of autism
What is PDA (Pathological Demand Avoidance)?
Ten things you need to know about Pathological Demand Avoidance
Does my child have Pathological Demand Avoidance?
The difference between PDA and ODD
Strategies for PDA (Pathological Demand Avoidance)
Pathological Demand Avoidance: Strategies for Schools
Challenging Behaviour and PDA
Is Pathological Demand Avoidance real?
Autism with demand avoidance or Pathological Demand Avoidance?
To follow me on other social media channels, you can find me at the following links or click the icons below!



















No comments:
Post a Comment
Comments are always very much appreciated and can really help the conversation go further...